- PEDS·DOC·TALK
- Posts
- The Most Measles Cases Since Eradication in the U.S.: What It Means for Kids, Travel, and Protection
The Most Measles Cases Since Eradication in the U.S.: What It Means for Kids, Travel, and Protection
From early vaccines to travel timing, here’s what parents are asking right now
We shouldn’t be here.
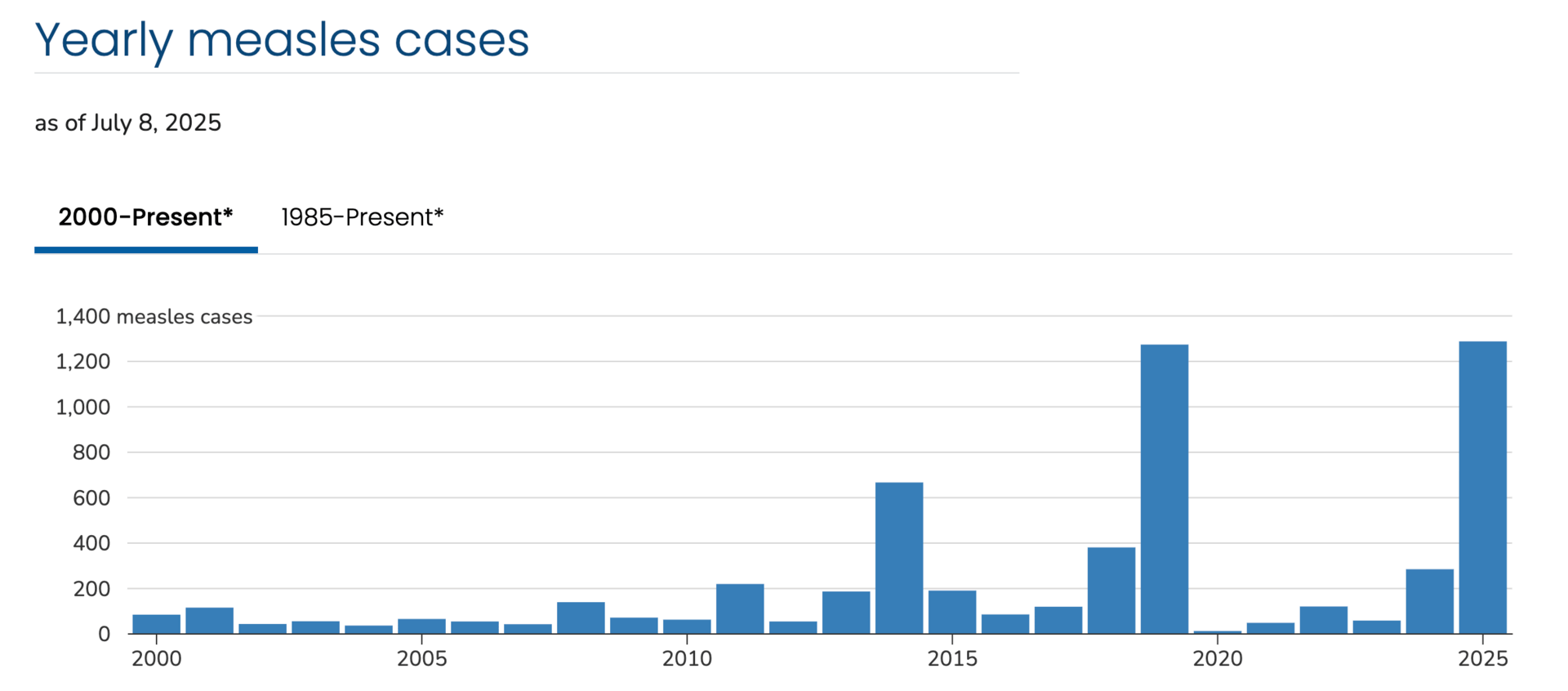
Measles has been making headlines again. As of the latest update in July 2025, 1,288 confirmed cases have been reported across 39 U.S. jurisdictions (see the link for recent updates).
That’s the highest number we’ve seen since measles was declared eradicated in 2000.
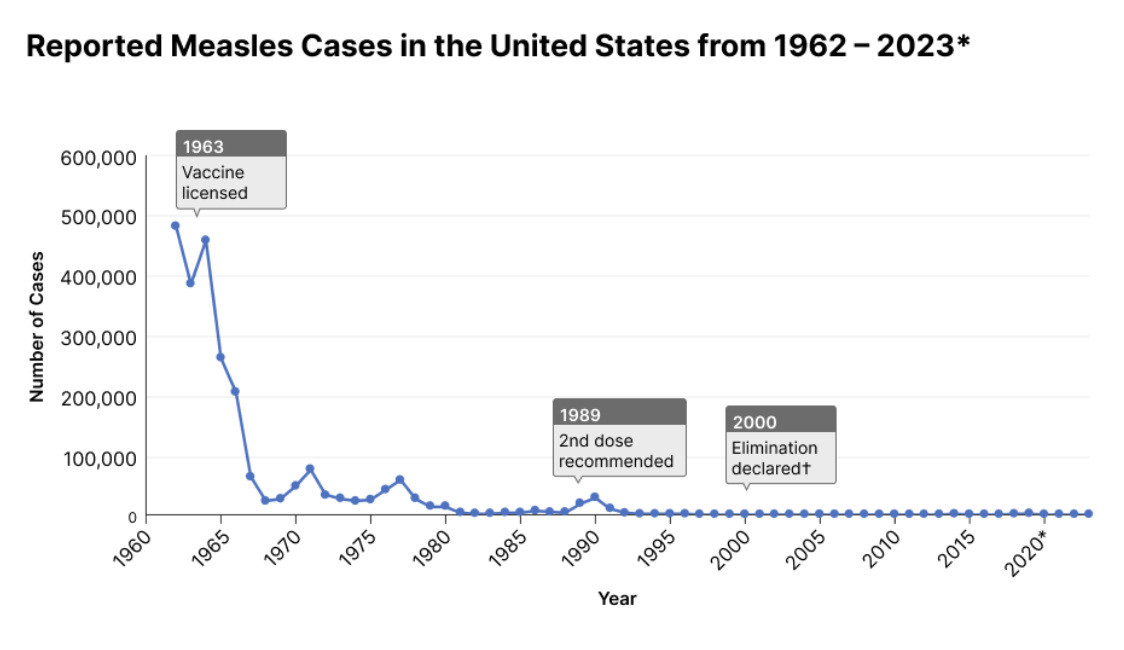
Eradication meant no continuous, local transmission for at least 12 months. A major public health milestone that showcased the power of science, vaccines, and collective action.
And yet, here we are. In recent years, cases have climbed-fueled by low vaccination rates in certain communities, often driven by misinformation and distrust.
It’s a deeply frustrating and heartbreaking setback. Not because we lack the tools to prevent it, but because we haven’t consistently used them.
Still, this isn’t a time for panic. It’s a time for clarity. The risks are real, but so is the protection we have.
If you’re preparing for summer travel, starting daycare or school, or just trying to make sense of the headlines, you’re not alone. Maybe your child is already vaccinated and you’re wondering if that’s enough. Or maybe your baby isn’t eligible yet, and you’re weighing whether to vaccinate early. These are thoughtful questions, and ones I’ve been hearing more and more.
Here’s what families are asking right now, along with the most up-to-date guidance to help you make informed, confident choices.
What’s happening with measles right now?
The U.S. is seeing a significant rise in measles cases this year. As of July 8, 2025, 1,288 confirmed cases have been reported across 39 jurisdictions, including states like California, Texas, Florida, Illinois, and New York. That’s more than four times the number of cases reported during all of 2024.
So what’s driving the increase?
Many of the current cases are linked to international travel and communities with low vaccination rates, but the ripple effects can reach far beyond those groups.
So far this year, the CDC has identified 27 measles outbreaks (defined as three or more connected cases), and 88% of total cases are part of those outbreaks. Places like airports, daycares, theme parks, summer camps, and schools are especially vulnerable when vaccination coverage drops, even slightly.
Why is measles so concerning?
It’s one of the most contagious viruses we know of. If someone infected walks into a room, the virus can linger in the air for up to two hours after they’ve left. And if you’re unvaccinated? There’s a 90% chance you’ll get sick after exposure.
The good news? Measles is preventable. Two doses of the MMR (measles, mumps, rubella) vaccine offer about 97% protection. And even if a vaccinated person does get infected, they typically have mild symptoms and are much less likely to spread it to others.
But we’re still seeing serious illness, especially in children.
Of the 1,288 confirmed U.S. cases in 2025:
29% have occurred in children under age 5
21% of those children have been hospitalized
And 3 deaths have been reported nationwide
In total, 13% of all cases have required hospitalization. And when we look at vaccination status, the story becomes clearer: 92% of confirmed cases were either unvaccinated or had unknown vaccine status.
That’s why many pediatricians, including myself, are having more conversations right now about early vaccination, travel precautions, and what families can do to protect babies who are too young for the routine MMR dose.
Because this isn’t about panic. It’s about preparation, clarity, and using the tools we have to reduce risk, especially for our youngest and most vulnerable.
Why are we seeing measles if it was “eradicated”?
You might remember hearing that measles was eradicated in the U.S. in 2000. Elimination means there’s no ongoing transmission within the country. In other words, we don’t have homegrown outbreaks year-round.
For years, the U.S. was able to prevent those travel-related cases from spreading widely, thanks to high vaccination coverage and strong public health infrastructure. But over time, that protection has slipped.
Here’s what’s changed:
The MMR vaccine coverage among U.S. kindergartners has dropped, from 95.2% in 2019–2020 to 92.7% in 2023–2024.
That drop leaves around 280,000 kindergartners unprotected, and that doesn’t include younger children, adults, or those with medical exemptions.
Even in states with high overall vaccination rates, there can be local pockets where many kids aren’t vaccinated, and that’s where outbreaks tend to spread quickly.
The MMR vaccine is very safe and highly effective, but it only works to stop outbreaks when enough people are protected. Public health experts generally aim for 95% coverage to achieve community immunity, because that level helps shield even those who can’t be vaccinated.
When coverage drops, even slightly, measles has more room to spread. And that’s what we’re seeing this year.
What parents are asking right now
Should I vaccinate my baby early for travel?
If you're traveling within the U.S. but not to an outbreak area, routine MMR vaccination at 12 months is still the standard recommendation. An early dose (6-11 months) is not routinely needed unless you’re going to a high-risk location. Here is how you might think through the decision more:
Any international travel
For travel within the U.S.
If no active outbreaks → No need for early vaccination.
If cases are rising but not declared an outbreak → Still no routine need, but be mindful of exposure risks in crowded places (airports, theme parks, etc.).
If you’re going to a declared outbreak area → Early vaccination at 6-11 months may be recommended (talk to your pediatrician).
Consider your baby’s exposure risks
Airports, public transportation, and crowded indoor spaces increase exposure risk, as measles spreads easily through the air.
If you’re staying with family or in low-risk settings, the risk is lower.
Understand what early vaccination means
If your baby gets an MMR dose at 6-11 months, they will still need two routine doses (one at 12 months, one at 4 years).
The early dose is helpful if exposure is likely, but if your travel is low-risk, it may not be necessary.
In summary, for domestic travel outside outbreak areas, the standard first MMR dose at 12 months is sufficient. If you have concerns about exposure, like traveling to a high-traffic tourist area or airport hubs, talk to your pediatrician about your baby’s specific risk and whether early vaccination is worth considering.
Some families may choose to get an early dose for travel, even if they’re not visiting a high-risk area-and that’s a decision best made in consultation with your child’s pediatrician.
If my child is over 1 and has had their first dose, do they need anything extra for travel?
No additional doses are needed for travel if they’ve already had their first routine dose at 12 months. If you’re traveling to a high-risk or outbreak area, you can talk with your pediatrician.
Can Vaccinated People Still Get Measles?
Rarely, but if they do, symptoms are typically mild and far less contagious than in unvaccinated individuals. The key takeaway? The MMR vaccine dramatically reduces both infection risk and severity.
How can I protect my newborn?
Babies under 1 year old are too young for routine MMR vaccination (albeit 6-12 months can receive it if internationally traveling, traveling to an outbreak area, or living in an outbreak area), so their best protection comes from limiting exposure, especially in outbreak areas. This includes crowded indoor places. Vaccinating those around your baby who are eligible is also great. For more on newborns and outings in general, watch this important video.
Here’s what helps:
Be mindful of your surroundings. Avoid unnecessary travel to outbreak areas and limit close contact with known unvaccinated individuals.
Check the caregiver's vaccination status. Ensure family members and caregivers are up to date on their MMR vaccine. This is the concept of herd immunity, where people who are unable to be vaccinated are protected by those who are vaccinated.
Consider early vaccination in outbreak areas. If you live in or are traveling to a high-risk area, your baby can get the MMR vaccine as early as 6 months old. This does not replace their routine doses at one and four years old.
Should I keep my kids home from daycare or school during an outbreak?
For fully vaccinated children (2 doses), there is no need to keep them at home, as they have strong protection (97%). However, if your child is too young to be vaccinated or immunocompromised, extra precautions may be necessary. Here’s how to approach the decision:
Ask if the facility has a measles vaccine policy. Do they require MMR vaccination for attendance? If they don’t, and there are unvaccinated children in the facility during an outbreak, your child’s risk of exposure is higher.
Consider the child’s age and vaccine status. If your child is not yet eligible for MMR or has received only one dose, their level of protection will differ:
What to do based on age & vaccination status
If your child is under 6 months (not eligible for MMR) → Highest risk since they have no direct protection. If there’s an outbreak in the daycare, consider temporary removal to avoid exposure.
If your child is 6-11 months and in an outbreak area → Early MMR vaccination is recommended. This early dose does not replace the routine doses at 1 & 4 years but provides temporary protection.
If your child is 1-4 years old and has received only one dose → A second (early) dose may be recommended if at least one month has passed since the first dose.
If your child is 4+ years old and fully vaccinated (2 doses) → No extra precautions needed. Their immunity is strong, and staying in school is safe.
If your child is fully vaccinated, the risk is low, but if they are too young to be vaccinated or only partially vaccinated, consider early vaccination or temporary removal in high-risk outbreak settings. Always consult with your pediatrician for personalized recommendations.
Want more answers?
From immunity testing to vaccine timing, the full Measles Q&A newsletter has it all. Plus, this PedsDocTalk YouTube video has more measles and virus answers.
Final thoughts
Measles outbreaks can feel scary, especially with headlines swirling and case numbers rising.
But this isn’t about panic. It’s about facts, options, and making informed choices for your family.
You do not need to barricade yourself indoors or fear that the moment you step outside, you or someone you love will catch measles.
The truth is: the MMR vaccine is highly effective, and its benefits far outweigh the risks. I strongly recommend it, as both a pediatrician and a mom. My own two children received their doses on schedule. As we prepare to travel internationally with our daughter, who’s had her routine first dose at 1 year, we’re choosing not to give the second dose early. But if she were under one? We would likely opt for the early dose.
When vaccine coverage stays high, it doesn’t just protect our own kids; it protects babies, immunocompromised individuals, and entire communities who depend on that shared immunity.
If your child is due for a dose, now is a good time to check in with your pediatrician. If you're traveling, ask about risks. And if you're unsure about your vaccine records or how to navigate these conversations, you’re not alone-we’re here to support you.
You’re already doing the most important thing: staying curious, staying informed, and showing up for your family. That matters more than ever.
If you enjoyed this newsletter, I’d love for you to share it with others! Screenshot, share, and tag me @pedsdoctalk so more parents can join the community and get in on the amazing conversations we're having here. Thank you for helping spread the word!
On The Podcast
If you’ve ever felt confused, judged, or overwhelmed by how weight is discussed at your child’s doctor’s visits? Whether your child is in a larger body, a smaller body, or somewhere in between this episode is for anyone who wants to raise healthy kids without harmful messaging.
I’m joined by Dr. Tommy Martin, a physician, educator, and passionate advocate for reframing weight and health conversations with compassion and clarity. Together, we explore why BMI was never meant to guide pediatric care, how weight bias shows up in medical settings, and what parents can do to protect their child’s body confidence without ignoring health.
Five and a half years ago, I became a mother. But the day my son was born wasn’t the best day of my life… it was the worst.
In this deeply personal Follow-Up episode, I revisit the story that changed everything for me: my traumatic birth experience with my son Ryaan, the complications that followed, and how it impacted me as a mother, a pediatrician, and a human.
Whether your birth went sideways slowly or spiraled in an instant—this episode is for you.
On YouTube
Worried about your baby’s weight percentile? Learn what growth charts really mean and when to worry (or not). This video includes
What is a percentile?
When to worry about percentiles?
How much weight should my baby be gaining?
What percentile is best?
What is growth faltering or failure to thrive?
Should I be concerned about weight fluctuations in baby?
When to worry about baby’s weight
How to support baby’s weight gain
Ask Dr. Mona
An opportunity for YOU to ask Dr. Mona your parenting questions!
Dr. Mona will answer these questions in a future Sunday Morning Q&A email. Chances are if you have a parenting concern or question, another parent can relate. So let's figure this out together!



Reply